As Life News reported on June 13, 2024:
“The Supreme Court on Thursday rejected a challenge to the abortion pill mifepristone, meaning the abortion drug will be widely available to continue killing babies and injuring doctors nationwide.
The 9-0 decision says the pro-life doctors who brought the case do not have standing – they were not injured, and so the court does not intervene. That’s even though they sued on behalf of women who were injured by the abortion drug by the thousands – including women who have been killed.” (Emphasis added)
The US Supreme Court decision acknowledged that the Mifeprex pill was approved in 2000 but also that:
“FDA placed additional restrictions on the drug’s use and distribution, for example requiring doctors to prescribe or to supervise prescription of Mifeprex, and requiring patients to have three in-person visits with
the doctor to receive the drug. ” (Emphasis added)
The Cout also acknowledges that the restrictions were relaxed further by the FDA (Federal Drug Administration) when:
“In 2021, the FDA announced that it would no longer enforce the initial in-person visit requirement. Four pro-life medical associations and several individual doctors moved for a preliminary injunction that would require the FDA either to rescind
approval of mifepristone or to rescind the FDA’s 2016 and 2021 regulatory actions. Danco Laboratories, which sponsors Mifeprex, intervened to defend FDA’s actions.”
Now as the Wall Street Journal reports:
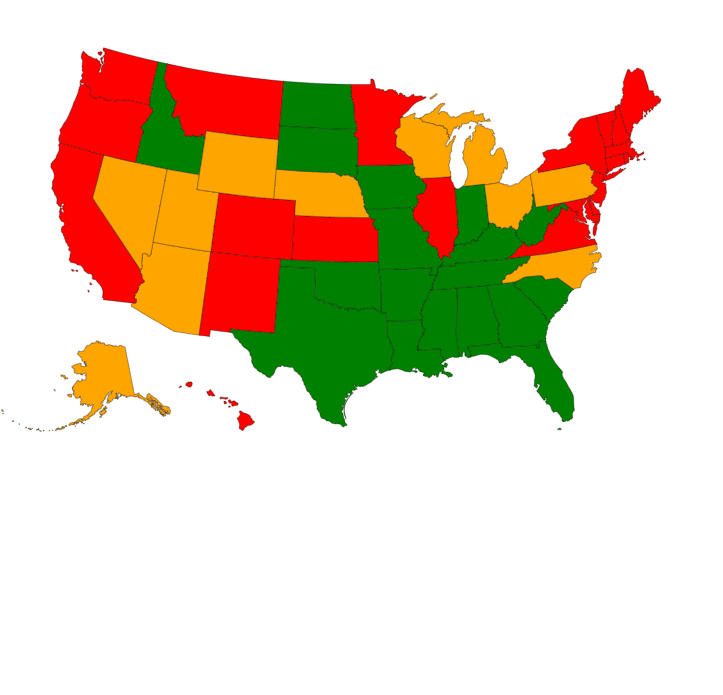
“Twenty-six states and D.C. allow telehealth for medication abortion. The remaining states have restrictions that supersede federal guidance: 14 ban abortion throughout pregnancy, and the remaining 10 have various combinations of in-person requirements, such as mandatory ultrasounds and visits to doctors and counselors.” (Emphasis added)
WHAT COULD GO WRONG?
As Dr. Christina Francis, an Ob-Gyn doctor herself, wrote in a May 2021 article titled “The government’s abortion pill policy puts mothers’ lives at risk”:
“One of the most significant reasons why an in-person visit has been required is for proper medical oversight as well as a physical exam and ultrasound. These visits are meant to accurately assess the gestational age of a woman’s pregnancy, as well as rule out ectopic pregnancy, which is life-threatening. The difference in size of an 8-week-old and 12-week-old preborn child is significant”
CONCLUSION
I have a personal interest in this because I had an unwed daughter who became pregnant and started bleeding without telling me because of embarrassment.
She went to a local ER where the doctors said she was just having a miscarriage and sent her home.
When the pain and bleeding increased, she called me. I took her back to the ER to demand an ultrasound.
As I suspected as a nurse, her pregnancy was ectopic and emergency surgery was performed.
Afterward, the surgeon showed me the picture he had taken (unasked) during the surgery to remove the then-deceased first-trimester baby, my grandchild. The picture was personally so sad to see but I was comforted that the surgeon cared enough to take a picture of this tiny person and show respect.
We need more respect and help for women with an unexpected pregnancy and their babies than a pill without medical safeguards!

You must be logged in to post a comment.